Abstract
Introduction:
Paroxysmal nocturnal hemoglobinuria (PNH) is a rare, life-threatening disease affecting 1-10 per million per year, characterized by uncontrolled complement-mediated intravascular hemolysis, thrombosis, and marrow failure. PNH manifests in a wide variety of symptoms such as fatigue, dyspnea, chest pain, abdominal pain, and hemoglobinuria. Due to its nonspecific presentation, patients may experience a delay in accurate diagnosis of this rare disease, which has been shown to have a significant impact on quality of life (QoL) and survival. At any point in the patient's journey, they may experience delays or poor accessibility to care. Key challenges in PNH remain its initial identification, diagnosis, and subsequent timely treatment.
Methods:
The Canadian PNH Network (CPNHN) use the "CATCH criteria'' to suspect diagnosis of PNH: Cytopenias, Aplastic anemia/myelodysplasia, Thrombosis, Coombs'-negative hemolysis, and Hemoglobinuria. This screening tool has not been formally validated, however it was hypothesized to be useful for real-world practitioners. In this study, we aimed to: (1) identify opportunities and gaps during the journey of a patient with suspected or confirmed PNH, referred to a CPNHN center (Pilot sites: University Health Network (UHN) & Sunnybrook Health Sciences Centre (SHSC)); (2) characterize time to diagnosis and treatment initiation, specifically considering CATCH criteria; and (3) assess the presentations with the highest frequency of being referred to a CPNHN center to create a process map.
Results:
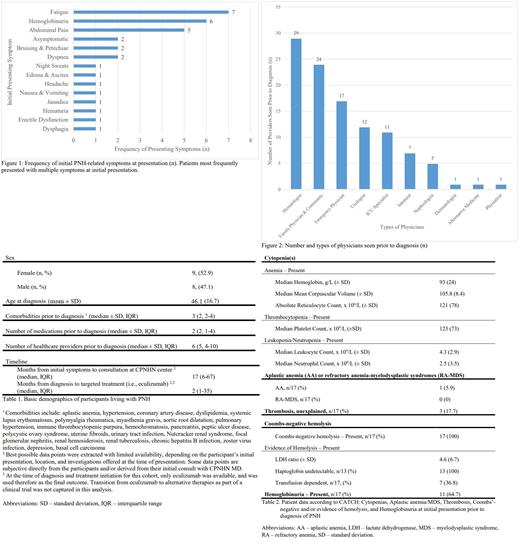
A total of 19 participants were identified at UHN, 17 charts were reviewed, and 15 patients were available for 30-minute individual interviews. The timeline was based on the participants' initial presentation to start of targeted treatment (i.e., eculizumab). Baseline demographic data are presented in Table 1. Mean age at diagnosis was 46.1 years (standard deviation [SD] 16.7), with varied symptoms at presentation (Figure 1). Median number of healthcare providers seen prior to diagnosis and/or referral was 6 (interquartile range [IQR] 4-10; Figure 2), and time from symptom onset to referral was 17 months (IQR 6-67). The most common CATCH criteria at presentation were hemoglobinuria, Coombs'-negative hemolysis, and cytopenias (i.e., anemia and thrombocytopenia) (Table 2). Flow cytometry revealed large granulocyte (85.9% ± 16.9), monocyte (84.7% ± 17.4), and type III RBC (20.8% ± 18.5) populations. From the interviews, we noted that individual participants had diverse experiences and journeys with PNH. Reflecting on the COVID-19 pandemic, participants reported no change in quality of care they had received, and some endorsed the convenience of virtual consultation without being required to travel long distances for in-person visits. Several suggestions included: improving community physician awareness and education on PNH, assistance with finances (transportation/parking), and need for ongoing patient education on available medications and clinical trials.
Discussion and Conclusion:
PNH is a rare disease that can manifest in many different, non-specific ways, contributing to delays in diagnosis and treatment initiation. We have characterized the patient journeys of a cohort of patients followed at our centers, and have identified gaps and potential areas for improvement. The variability and delay in assessment for PNH may be attributed to the diverse backgrounds of the participants, first presentation abroad, year of symptom presentation, and availability of high-sensitivity flow cytometry, which is the diagnostic gold standard. In addition to characterizing the initial presentations and barriers to diagnosis and treatment, we also evaluated humanistic factors such as QoL. As PNH is rare, the study was limited by the small sample size and some incomplete records, as some patients were diagnosed and managed elsewhere initially.
We plan to expand our work across Canada, which will increase our cohort size and better allow an assessment of the impact of geographical differences on access to care. Following this, we plan to provide recommendations for diagnostic and treatment benchmarks to colleagues across the country, introduce the CATCH criteria, and subsequently evaluate the impact of these knowledge translation strategies with comparison to our initial cohort.
Chow: Alexion: Other: Site investigator for clinical trial. Patriquin: Alexion, AstraZeneca Rare Disease: Consultancy, Honoraria, Speakers Bureau; Apellis: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Biocryst: Honoraria; Sanofi: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal